In an era where precision and efficiency are essentials, the many benefits of e-prescribing have emerged as a game-changer for medication management. By allowing healthcare providers to generate and transmit prescriptions electronically it eliminates risks tied to traditional paper methods, which leads to miscommunication and illegibility. This shift toward digital solutions is evident—recent reports value the global e-prescribing market reaching $26.17 billion by 2032.
When integrated with Electronic Health Records (EHR) system, e-prescribing enhances clinical decision-making by providing real-time access to patient data like allergies and medication histories. This connection reduces delays and fosters stronger collaboration between providers and pharmacies, leading to safer and more efficient care delivery. This blog will in-depth break down the same sections, wherein we’ll describe the benefits of e-prescribing and how its integration with EHR systems transforms healthcare operations and patient outcomes.
Understanding E-Prescribing: What It Is and Why It Matters?
E-prescribing, or electronic prescribing, is a digital method of creating and sending prescriptions directly to pharmacies, replacing handwritten paper slips.
By using a computer-based system, healthcare providers can ensure prescriptions are clear, accurate, and free from the errors that often result from illegible handwriting or miscommunication. This technology streamlines the prescribing process, reducing delays and improving patient safety.
The impact and benefits of using e-prescribing are undeniable. In 2024, over 95% of U.S. hospitals have adopted EHR systems, underscoring their critical role in the healthcare infrastructure. At the core of e-prescribing lies its seamless integration with Electronic Health Records (EHR)—a digital record of a patient’s medical history. This connection gives providers real-time access to critical patient information, such as allergies and previous medications, enabling informed decisions that enhance care quality and operational efficiency.
As healthcare development embraces digital solutions, e-prescribing stands out as a key innovation for safer and more streamlined care. It has become more than just a convenience—it’s a tool that redefines safety, efficiency, and outcomes. Let’s look closer at the key benefits of using e-prescribing and how it enhances patient safety and care.
Related reading: What is EHR System and How to Build It? – Guide and Process
Key Benefits of E-Prescribing: Enhancing Patient Safety and Care
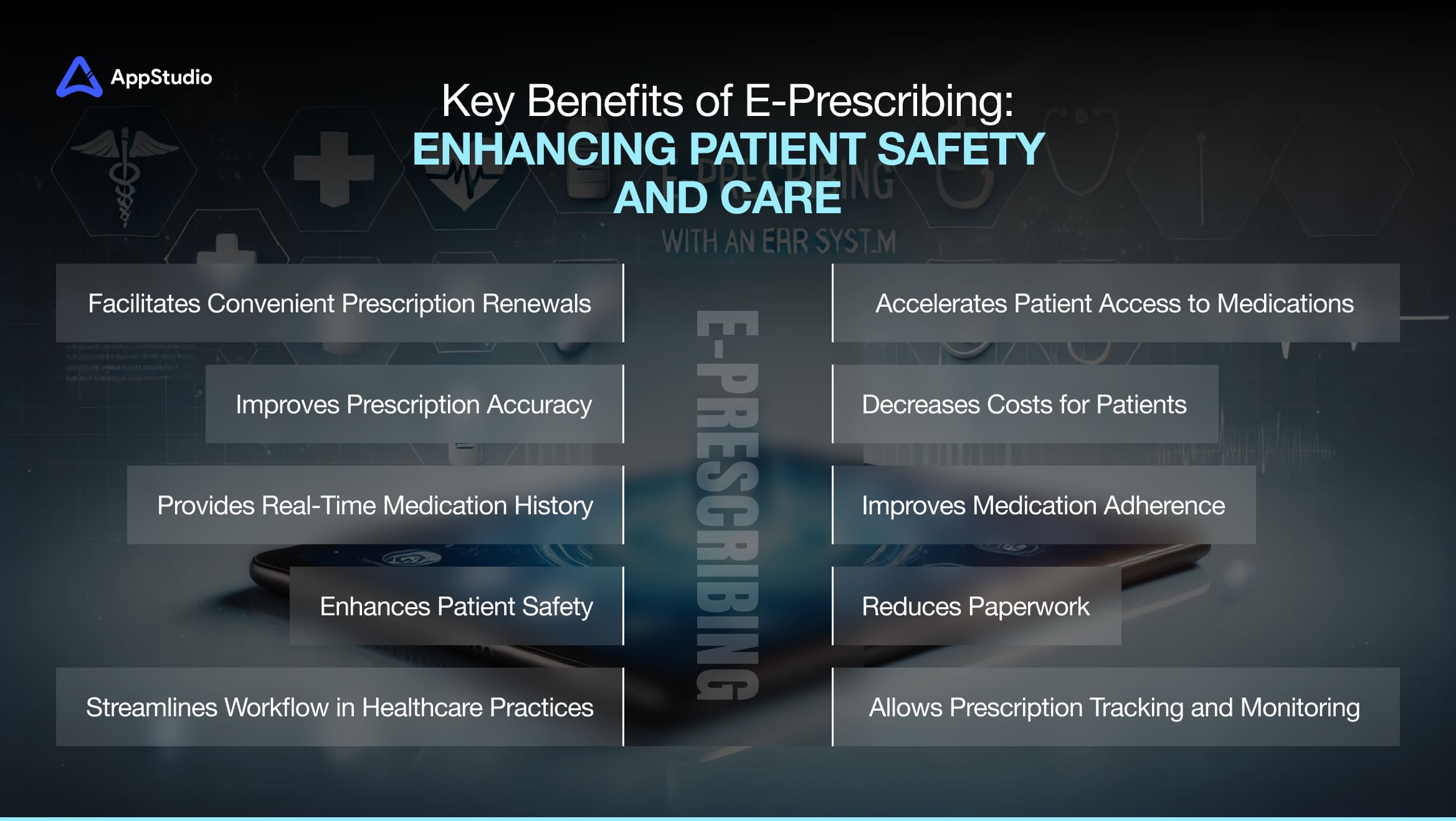
In a healthcare environment where every detail matters, e-prescribing has emerged as a solution that bridges efficiency and safety. As we describe the benefits of e-prescribing, it’s clear that it fundamentally improves how medications are managed and delivered.
1. Enhances Patient Safety
E-prescribing eliminates the risks associated with illegible handwriting and miscommunication that come with paper prescriptions. By sending prescriptions digitally, healthcare providers ensure accuracy, while built-in alerts notify clinicians about potential drug interactions or patient allergies. This real-time process helps explain the benefits of e-prescribing and significantly reduces medication errors, making patient care safer.
2. Improves Prescription Accuracy
Accuracy is at the core of e-prescribing. Features like automated dosage calculations, standardized drug databases, and precise digital entries minimize human errors during the prescribing process. This ensures patients receive the correct medications in the proper dosages as intended by their healthcare providers.
3. Provides Real-Time Medication History
E-prescribing integrates seamlessly with Electronic Health Records (EHR) to provide instant access to a patient’s complete medication history. Clinicians can view current prescriptions, past treatments, and potential risks in real-time, ensuring that any new medication prescribed is appropriate and safe for the patient’s overall health profile.
4. Streamlines Workflow in Healthcare Practices
E-prescribing automates routine prescription tasks, saving providers time. The need for manual processes like writing, calling, or faxing pharmacies is eliminated, allowing clinicians to focus more on patient care. This streamlined workflow boosts productivity and enhances service delivery across healthcare settings.
5. Facilitates Convenient Prescription Renewals
Prescription renewals can often be time-consuming for both patients and providers. E-prescribing simplifies this process by allowing patients to request refills electronically through patient portals or mobile apps. The added conveniences explain the benefits of e-prescribing and ensure patients manage their medications effortlessly, improving satisfaction and adherence.
6. Accelerates Patient Access to Medications
E-prescribing reduces patient waiting times by transmitting prescriptions directly to pharmacies. This is particularly crucial for individuals needing immediate treatments or managing chronic conditions. Faster access to medications ensures timely treatment, supporting better health outcomes.
7. Allows Prescription Tracking and Monitoring
E-prescribing enables healthcare providers to monitor when prescriptions are filled or refilled electronically. This real-time tracking helps identify missed doses, medication misuse, or adherence issues early on. Providers can then intervene proactively to support patients and ensure therapies are followed as prescribed.
8. Improves Medication Adherence
E-prescribing simplifies the prescription process by removing manual handling of physical slips. Features like automated reminders for refills sent through patient portals or apps ensure patients stay on track with their medications. Higher adherence rates lead to improved health outcomes, particularly for those managing long-term conditions.
9. Decreases Costs for Patients
With access to real-time insurance and formulary information, providers can recommend cost-effective medication alternatives that align with a patient’s insurance plan. This reduces out-of-pocket expenses and encourages adherence by removing financial barriers to treatment.
10. Reduces Paperwork
Transitioning to digital prescriptions eliminates the need for physical documentation. This reduces administrative burden, minimizes storage needs, and declutters medical offices. Staff can focus more on delivering care than managing stacks of paperwork, creating a more efficient healthcare environment.
These key features and benefits of using e-prescribing software set the foundation for safer and more efficient healthcare workflows. However, they function effectively only when supported by a well-designed system with essential components. Let’s explore the core components furthermore that enables e-prescribing systems to deliver on their promise of accuracy, security, and efficiency.
Related reading: Pros and Cons of Customizing Your EHR
Standard Components of an Electronic Prescription System

Understanding the core components of an effective e-prescribing system is crucial to ensuring its successful implementation. Below are a few functions to look out for.
1. User Authentication and Access Control
E-prescribing systems rely on secure user authentication to ensure only authorized healthcare providers can access and operate the system. This often includes multi-factor authentication (MFA) for an added layer of security.
Why It Matters: Secure access prevents unauthorized use, protects sensitive patient information, and ensures compliance with privacy regulations like HIPAA. It reduces the risk of data breaches, safeguarding patient trust and organizational integrity.
2. Accurate Patient Identification and Data Access
The system must enable providers to identify patients accurately and access their complete medical records, including medication history, allergies, and ongoing treatments.
Why It Matters: Correct patient identification is critical to avoiding medication errors. By accessing comprehensive health records, providers can make informed decisions and prescribe medications that align with the patient’s health needs.
3. Seamless Interoperability
Interoperability ensures that e-prescribing systems can seamlessly connect with other healthcare IT platforms, such as Electronic Health Records (EHRs) and hospital management systems.
Why It Matters: Interoperability in healthcare facilitates smooth information exchange and enhances communication between healthcare providers, pharmacists, and other stakeholders. This leads to coordinated care, fewer errors, and better patient outcomes.
Key Features of E-Prescribing Software
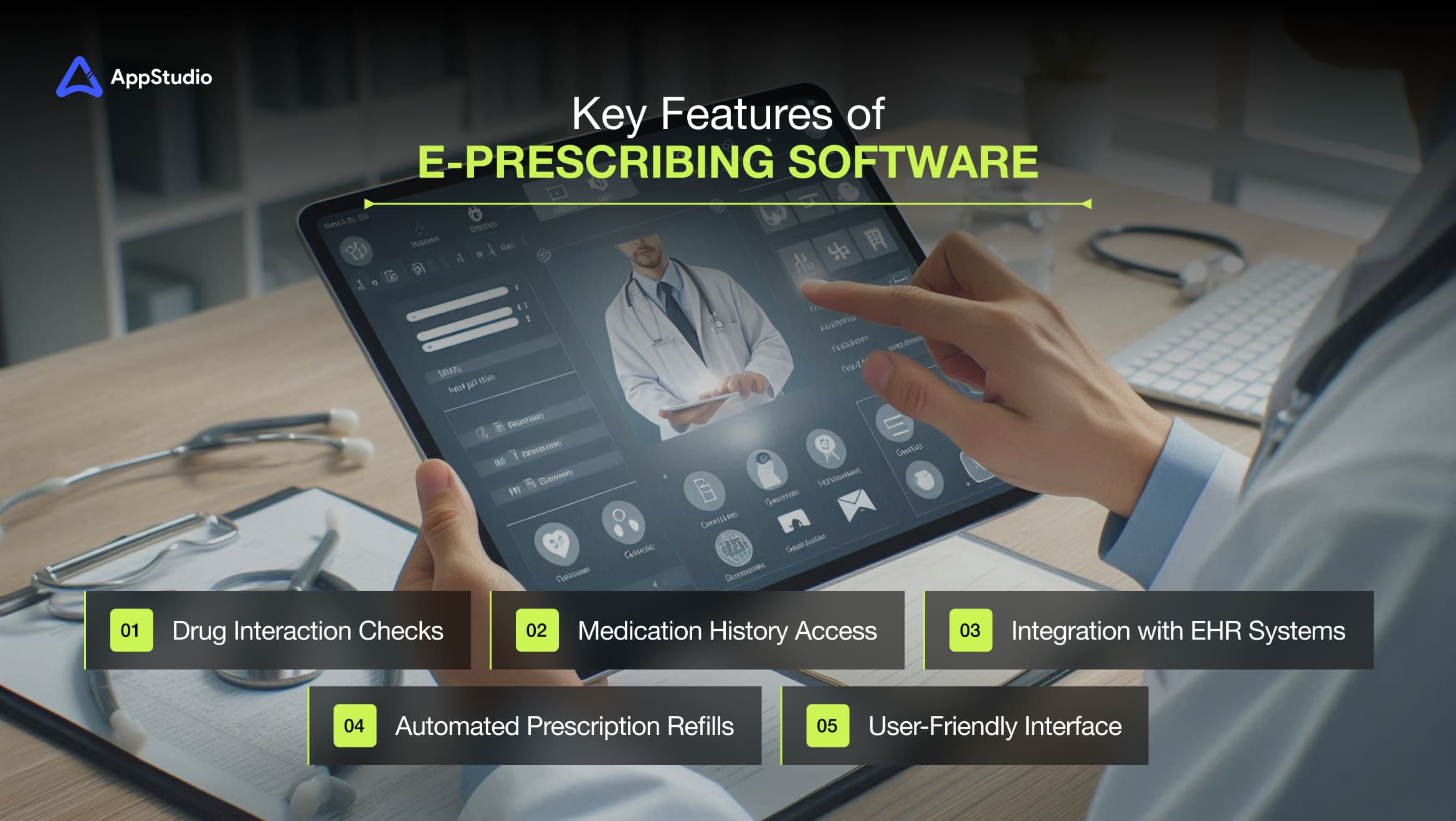
The true power of e-prescribing software lies in its features, making it efficient, accurate, and user-friendly for healthcare providers and patients. Here are some of its go-to key features:
1. Medication History Access
When you E-prescribing software provides healthcare providers immediate access to a patient’s complete medication history. This includes details of past prescriptions, adherence patterns, and treatment changes over time. By pulling data from integrated systems, providers can review a clear, real-time view of medications without relying on scattered records or manual documentation.
Why It Is Important: Access to this history prevents adverse drug interactions, identifies gaps in treatment, and ensures safer prescribing decisions. It allows providers to avoid duplications and confidently prescribe medications that align with patients’ health needs.
2. Drug Interaction Checks
This feature acts as a built-in safety net within e-prescribing software. As providers input a prescription, the system automatically scans for potential drug interactions, allergies, or contraindications based on the patient’s medical profile. These alerts are presented in real-time, ensuring immediate action.
Why It Is Important: Drug interaction checks play a critical role in enhancing patient safety by flagging risks before prescriptions are finalized. This helps prevent adverse reactions leading to serious health complications, improving overall treatment reliability.
3. Automated Prescription Refills
E-prescribing software streamlines the refill process by allowing patients to submit requests electronically through apps or patient portals. Once approved, prescriptions are automatically updated and sent to the pharmacy, eliminating manual back-and-forths.
Why It Is Important: This automation ensures patients always have access to their medications without unnecessary delays. It reduces the administrative burden on clinics, improves medication adherence, and makes managing chronic conditions easier for patients.
Related reading: Top EHR Features and Their Impact on Healthcare
4. Integration with EHR Systems
E-prescribing software seamlessly integrates with Electronic Health Record (EHR) systems, allowing real-time patient health data updates. Prescriptions, medical history, and treatment plans are unified under one digital platform, creating a single source of truth for clinicians.
Why It Is Important: This integration enhances communication between healthcare providers and pharmacies, improving care coordination. Real-time updates also allow clinicians to make informed decisions without delays, improving accuracy and patient outcomes.
5. User-Friendly Interface
A user-friendly interface prioritizes intuitive navigation, ensuring healthcare providers can efficiently use the system with minimal training. Features like quick access menus, smart search options, and simple workflows allow smoother operations.
Why It Is Important: An easy-to-use system leads to faster adoption, fewer errors, and improved productivity. Clinicians can spend less time on technical hurdles and focus more on patient care, ultimately enhancing workflow efficiency.
E-Prescription Adoption: A Then & Now Comparison
The adoption of electronic prescribing has transformed how healthcare providers manage prescriptions, improving workflow efficiency, patient engagement, and medication safety. Here’s a comparison of key areas where this technology has significantly impacted.
1. Integration with Healthcare IT Systems
Before E-Prescription Adoption: Healthcare systems operated in silos, making it difficult for providers to access complete patient records during the prescribing process. Medication histories were often incomplete, increasing the risk of adverse drug interactions and treatment inefficiencies.
After E-Prescription Adoption: E-prescribing systems seamlessly integrate with Electronic Health Records (EHR) and other healthcare IT platforms, providing real-time access to a patient’s comprehensive medication history. This integration supports informed clinical decisions, reduces errors, and ensures prescriptions align with the patient’s current treatment plan.
2. Workflow Efficiency
Before E-Prescription Adoption: Traditional prescription methods were time-consuming and inefficient. Providers manually wrote prescriptions, often leading to communication delays with pharmacies via phone or fax. This not only slowed down the dispensing process but also burdened healthcare staff with repetitive administrative tasks.
After E-Prescription Adoption: E-prescribing has streamlined the workflow by enabling providers to send prescriptions electronically to pharmacies. This eliminates manual steps, reduces errors, and dispenses medications quickly. As a result, healthcare providers can dedicate more time to patient care than administrative duties.
3. Prescription Accuracy
Before E-Prescription Adoption: Handwritten prescriptions were often misinterpreted due to illegible handwriting or unclear instructions. Pharmacists had to rely on guesswork or contact providers for clarification, increasing the risk of medication errors and delays that could compromise patient safety.
After E-Prescription Adoption: E-prescribing eliminates ambiguity by electronically generating precise, standardized prescriptions. According to a 2024 study, prescribing errors decreased from 1.43% to 0.51% after implementing e-prescription systems, significantly improving accuracy. This reduction ensures pharmacists receive precise details every time, minimizing the chance of errors and ensuring patients receive the correct medications and dosages.
The adoption of e-prescribing has revolutionized how prescriptions are managed, improving patient safety and operational efficiency across healthcare systems. This upward trend shows no signs of slowing down. In 2021, 94% of all prescriptions in the United States were filled electronically, up from 84% in 2020 and 80% in 2019. As healthcare providers prioritize digital solutions, adopting e-prescribing systems will only grow, cementing their role as a cornerstone of modern, efficient, and error-free patient care.
Related reading: Types of Electronic Health Record (EHR) Systems
Wrapping Up!
To Adopt and to describe the benefits of e-prescribing is no longer just an upgrade— it’s improving accuracy, patient safety, and operational efficiency in healthcare is necessary. AppStudio specializes in building tailored, cutting-edge healthcare solutions that seamlessly integrate e-prescribing features with your Electronic Health Record (EHR) systems. Our expert team ensures secure, user-friendly platforms that meet regulatory standards and drive real-world results for healthcare providers and patients.
Whether you’re looking to implement a new e-prescribing system or optimize your existing infrastructure, AppStudio is here to guide you every step of the way. Let us help you transform your healthcare operations and deliver more intelligent, safer patient care.
Book a free consultation today to discover how our solutions can streamline your workflows and position your healthcare practice for success!
Frequently Asked Questions
E-prescribing is a digital system that allows healthcare providers to create and send prescriptions electronically to pharmacies. This eliminates paper-based errors and speeds up the prescribing process, ensuring accuracy and efficiency.
E-prescribing reduces medication errors, improves workflow efficiency, and enhances patient adherence to prescribed treatments. It also helps providers screen for drug interactions, allergies, and other risks, making the medication process safer and cost-effective.
Yes, e-prescribing software is secure and HIPAA-compliant. It uses encryption and secure networks to protect patient data during transmission, ensuring privacy and preventing unauthorized access.
Yes, most e-prescribing systems are designed to integrate seamlessly with EHR systems. This integration provides real-time access to patient information, medication histories, and treatment plans, allowing healthcare providers to make well-informed decisions.
AppStudio delivers customized e-prescribing solutions that meet healthcare providers’ unique needs. Our secure, scalable systems integrate seamlessly with existing EHR platforms, ensuring efficient workflows, enhanced patient safety, and improved operational outcomes.