Remember when hospitals were buried under piles of paperwork? Thankfully, those days are long gone. With the rise of EHR system development, the industry has solved many of healthcare’s biggest challenges, benefiting patients, practitioners and providers alike.
EHR systems not only eliminate the need for physical files but also automate many aspects of healthcare management. They are critical in improving patient outcomes by streamlining administrative tasks, enhancing patient care, and ensuring secure data access. In fact, recent projections suggest that the global EHR market is expected to hit USD 52.98 billion by 2027.
Building an EHR system might sound complex, but with the right tools, team and services, it’s easier than ever. This blog will take you through a head-to-toe guide to the EHR system development process.
What is EHR?
An Electronic Health Record (EHR) is a digital version of a patient’s paper chart, capturing everything from medical history, diagnoses, and medications to treatment plans, immunization dates, and lab results. This summary is stored and shared using specialized software, allowing healthcare providers to track patient information over time and coordinate care more effectively. Whether it’s physicians, labs, pharmacies, or even the patients themselves, EHR systems ensure that all authorized individuals involved in the patient’s care can access and share important medical data.
Notably, it’s easy to confuse Electronic Health Record Development (EHR) with Electronic Medical Records development (EMR); the two terms are often used interchangeably. The main distinction lies in their scope.
- While EMR is focused on a specific clinic’s data
- EHR offers a broader view, allowing for the seamless exchange of information across multiple healthcare facilities.
Simply put, EHR systems help healthcare providers keep track of everything, ensuring no critical details are overlooked while making the process smoother and less time-consuming.
Related reading: What Is Interoperability in Healthcare? – A Complete Guide
Types of EHR Systems
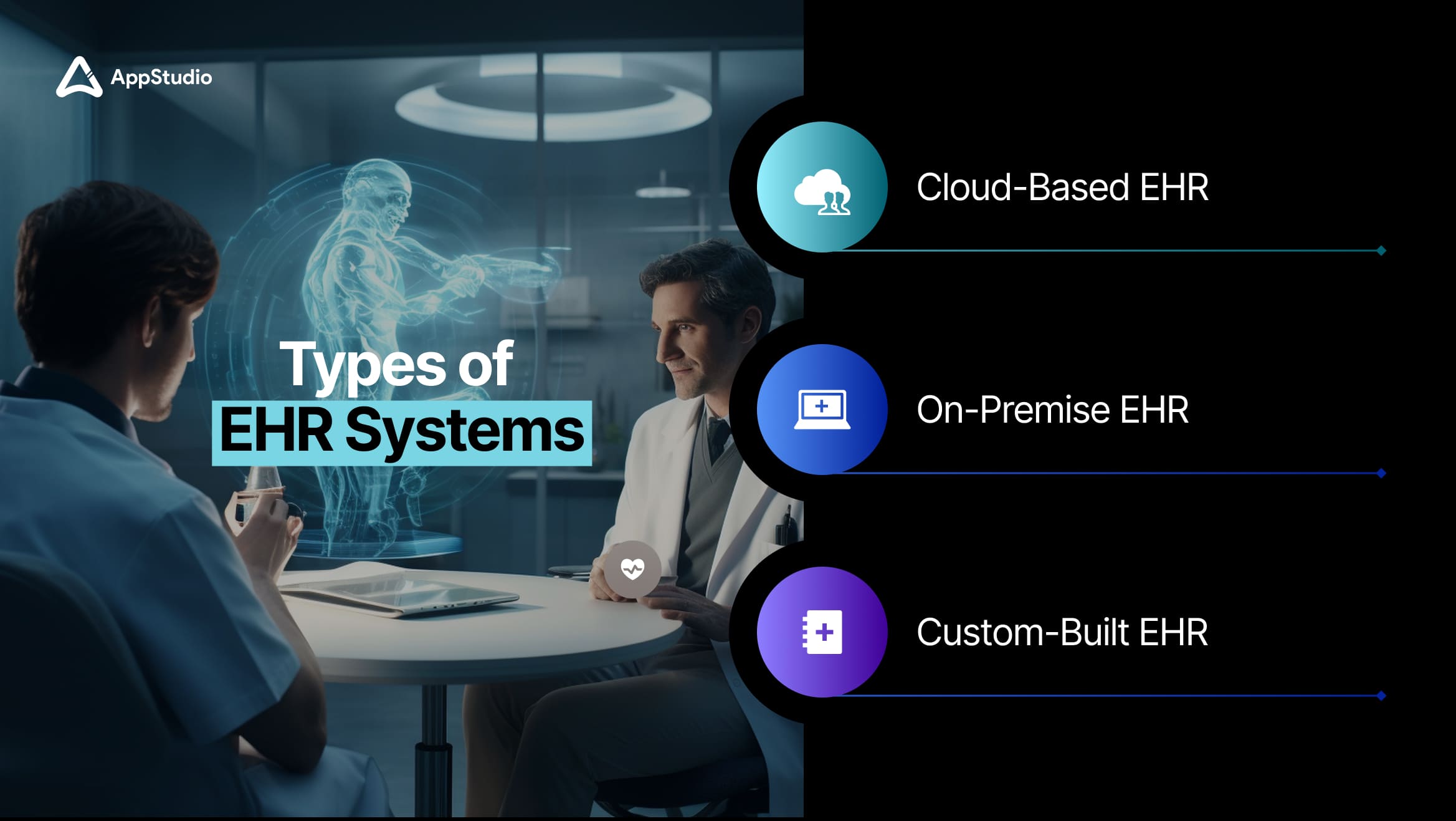
When choosing an EHR system, healthcare providers have several options to consider. Each type offers distinct advantages depending on multiple factors. Here are the different types of EHR systems and how they benefit both healthcare providers and patients.
1. Cloud-Based EHR
A cloud-based EHR is hosted on remote servers and accessed via the Internet, providing a high degree of flexibility and scalability. Since the data is stored in the cloud, there’s no need for expensive on-site hardware, making it ideal for small—to medium-sized practices with limited IT resources.
Benefits
- Lower upfront costs
- Automatic updates
- Accessibility
2. On-Premise EHR
An on-premise EHR is installed locally on the healthcare provider’s servers, giving organizations greater control over their data and systems. This type of EHR is typically used by larger healthcare organizations with the necessary IT infrastructure and can handle the higher upfront costs and ongoing maintenance requirements.
Benefits
- Greater control over data
- Customization
- No reliance on Internet connectivity
3. Custom-Built EHR
A custom-built EHR is designed from the ground up to meet an organization’s specific needs. While this option can be more expensive and time-consuming, it offers unparalleled flexibility and can be fully integrated with existing systems and workflows.
Benefits
- Tailored to specific needs
- Integration flexibility
- Scalability
Type of Tech Stack Required to Build an EHR System

During the building of a robust EHR system development, choosing the right technology stack is critical to ensuring seamless performance, scalability, and security. The healthcare industry demands systems that can handle vast amounts of sensitive data while offering high availability, fast processing, and compliance with stringent regulations like HIPAA.
Let’s explore the key technical components involved in EHR software development.
1. Front-End Technologies
The front end of an electronic health record development is what healthcare providers, administrators, and patients interact with primarily, so the design must prioritize ease of use, responsiveness, and intuitive navigation. A well-designed interface ensures that healthcare professionals can focus on patient care rather than struggling with the software.
Key Frameworks: React and Angular
- React: React is often preferred for building highly responsive interfaces with dynamic updates. For instance, a doctor needs real-time updates on a patient’s lab results or vitals during a consultation in an electronic health record system development. React’s component-based architecture enables the creation of highly modular and reusable UI components, making it easy to manage complex workflows within the EHR.
- Angular: Angular is another powerful framework that excels in building large-scale applications. It offers two-way data binding, meaning any updates made in the UI (e.g., new treatment records) are immediately reflected in the back end. Angular’s templating capabilities and strong TypeScript support make it ideal for building complex, enterprise-grade healthcare solutions.
2. Back-End Technologies
The Back end of an EHR system is where all patient data is stored, processed, and retrieved. Given the sensitivity of healthcare data, the back-end must be reliable, scalable, and secure, capable of handling high data loads and ensuring fast access to critical medical records.
Database Management Systems (DBMS)
- MongoDB: Known for its scalability and flexibility, MongoDB is often used in EHR systems where unstructured or semi-structured data (e.g., notes from consultations and diagnostic images) needs to be stored efficiently. Its NoSQL structure allows for rapid querying of large datasets, which is especially important in environments with growing patient databases.
- MySQL: MySQL is a reliable relational database management system, often used in healthcare settings for structured data like patient demographics, appointment schedules, and treatment histories. Its ACID-compliant nature ensures data integrity, making it the backbone of many EHR software development projects where consistency and transactional safety are paramount.
Server-Side Frameworks
- Node.js: Often paired with MongoDB, Node.js development allows for fast, non-blocking data processing, making it a great choice for healthcare systems requiring high concurrency, such as handling thousands of patient records in real time.
- Python with Django: Python’s Django framework is often chosen for EHR systems requiring complex workflows and extensive business logic. It offers rapid development with built-in tools for handling security (like authentication) and database operations.
3. Security Measures
In healthcare, security is not just an important feature—it is a legal obligation. With healthcare data breaches reaching record levels in 2023 and exposing millions of patient records, robust security measures are non-negotiable. According to recent data, the healthcare industry witnessed over 700 breaches in 2023 alone, highlighting the growing threat to medical data.
Key Security Features:
- Encryption: AES-256 encryption is commonly used for securing both data at rest (in databases) and data in transit (being transferred between systems).
- Multi-Factor Authentication (MFA): Given the sensitivity of healthcare data, MFA adds a layer of protection by requiring users to verify their identity using two or more methods ( password + OTP).
- Role-Based Access Control: RBAC ensures that only specific individuals within the healthcare organization can access certain types of information. For example, a nurse might have access to basic patient records but not financial or sensitive treatment data.
- HIPAA Compliance: HIPAA (Health Insurance Portability and Accountability Act) compliance is mandatory for any EHR system operating in the US. It outlines strict requirements for data encryption, access controls, audit trails, and more, ensuring the privacy and security of patient information. Non-compliance can result in significant legal penalties and reputational damage.
Related reading: Top 10 Mobile App Features in Healthcare
Team Required to Build an EHR Software
Building an in-place electronic health record system development isn’t just about writing code. It’s a multifaceted process that requires collaboration between various professionals, each playing a crucial role in bringing the project to life. Let’s break down the roles required and why each is indispensable.
1. Project Manager
The Project Manager is the backbone of the EHR development process. They act as the glue between the client (in this case, healthcare providers) and the development team. They oversee the project from start to finish, ensuring every milestone is met on time and within budget.
Key Responsibilities:
- Planning & Coordination
- Stakeholder Communication
Why It’s Crucial: Healthcare projects, especially EHR software, are highly sensitive due to the data privacy and compliance requirements involved. A strong PM ensures that the project adheres to regulations like HIPAA while meeting the healthcare provider’s expectations. Without solid project management, timelines can easily slip, and the software can fall short of industry standards.
2. Software Developers (Front-End and Back-End)
Your software developers are the builders of the EHR system development, responsible for creating the application’s front-end (what the users see and interact with) and back-end (where the data is stored and processed) components.
Key Responsibilities:
- Front-End Development
- Back-End Development
Why It’s Crucial: The success of an EHR system hinges on seamless performance and data accessibility. If the front end is clunky or slow, doctors and nurses won’t use it. The system risks violating privacy laws and damaging trust if the back-end doesn’t securely manage vast amounts of sensitive data. Your development team is the project’s core, ensuring that the EHR software is reliable and user-friendly.
3. UX/UI Designers
UX/UI designers are pivotal in how effectively healthcare providers will use the electronic health record system development. Doctors, nurses, and administrative staff need to access patient data quickly and efficiently in a fast-paced clinical setting. A poorly designed user interface can lead to frustration, errors, and time wasted navigating the software.
Key Responsibilities
- User Experience (UX) Design
- User Interface (UI) Design
Why It’s Crucial: Even minor delays or confusion in accessing information can affect patient care in healthcare. A well-designed EHR system can drastically reduce the time it takes to locate patient records, document treatments, and share information across departments. Your UX/UI designers ensure the system is easy to navigate, increasing its overall adoption among healthcare staff.
4. Quality Assurance (QA) Testers
No software launch is complete without rigorous testing. QA testers ensure the EHR system functions as intended, without bugs or performance issues. Since EHRs deal with sensitive patient information, the system must be thoroughly tested to avoid data breaches, crashes, or slowdowns.
Key Responsibilities:
- Functional Testing: QA testers ensure that all features work as expected. For instance, they check whether a doctor can retrieve a patient’s medical history without delays or if the system accurately records and saves updates in real-time.
- Security Testing: They verify that the system meets compliance standards like HIPAA, ensuring patient data is secure. This involves testing encryption protocols, access controls, and user authentication processes to protect sensitive health information.
- Performance Testing: EHR system development often use large datasets, especially in hospitals. QA testing simulate heavy data loads to ensure the system remains fast and responsive, even under pressure.
Why It’s Crucial: There’s no room for error in healthcare. A malfunctioning EHR can lead to misdiagnoses, treatment delays, or worse. QA testers ensure that the software is secure, reliable, and ready for deployment, giving healthcare providers the confidence to trust the system.
5. Compliance and Security Experts
Given the highly regulated nature of healthcare, compliance and security experts are critical team members. Their role is to ensure that the EHR system adheres to all local and international regulations regarding data protection, like the Health Insurance Portability and Accountability Act (HIPAA) in the US or the GDPR in Europe.
Key Responsibilities
- Compliance Audits
- Security Protocols
Why It’s Crucial: A data breach or non-compliance with healthcare regulations can lead to hefty fines, legal trouble, and loss of trust. Security and compliance experts ensure that your EHR software works well, keeps patient data safe, and meets all legal requirements.
6. Healthcare Consultant
A healthcare consultant bridges the gap between the technical team and the healthcare provider. They bring industry-specific insights and ensure that the software aligns with the actual needs of medical professionals. They provide feedback on workflows, data capture methods, and clinical requirements to ensure the system integrates seamlessly into a healthcare setting.
Key Responsibilities:
- Workflow Optimization: They ensure that the software complements the day-to-day operations of healthcare providers, making processes more efficient without introducing unnecessary complexity.
- Clinical Insights: Healthcare consultants advise on key features medical staff need, such as how lab results should be displayed or how patient histories should be organized.
Why It’s Crucial: Developers might not always have in-depth knowledge of the healthcare industry, and this can result in a system that doesn’t fully meet the needs of doctors or nurses. A healthcare consultant ensures the EHR system is built from a clinical perspective, maximizing its usefulness in real-world scenarios.
Related reading: How is IoMT Revolutionizing the Healthcare Industry?
Steps to Build an EHR System
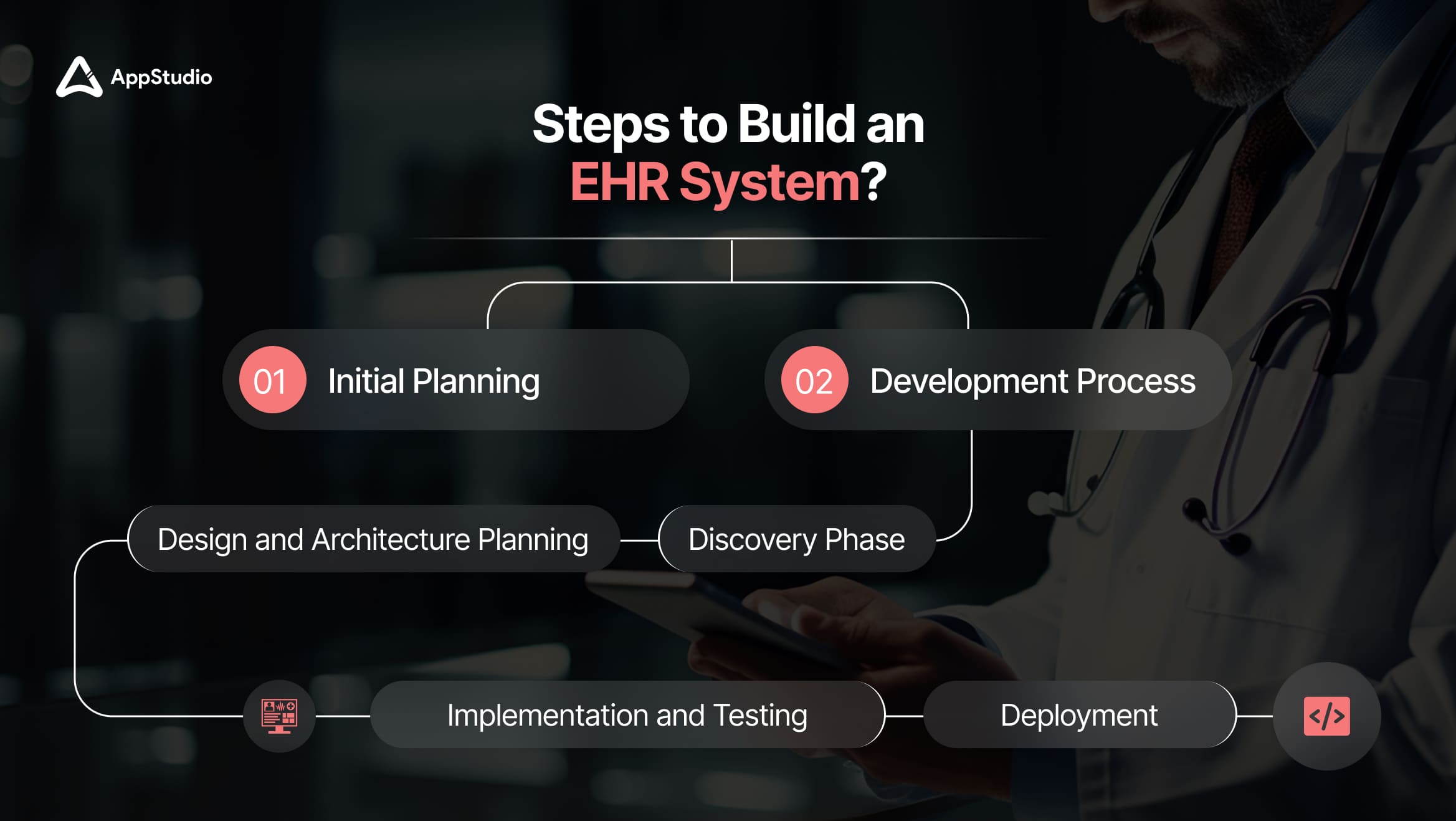
An EHR system development involves several key steps, each critical to ensuring the system is functional, compliant, and user-friendly. Here’s a roadmap to follow:
1. Initial Planning
Before any coding begins, it’s essential to define the goals and objectives of the electronic health record system development. Thus, asking these questions is imperative to set up an initial plan.
- What specific challenges does the healthcare provider want to address?
- Are there unique workflows or regulatory requirements that need to be integrated?
This phase also involves gathering input from stakeholders to create a detailed blueprint for development.
2. Development Process
- Discovery Phase: A thorough analysis of the healthcare provider’s workflows and needs is conducted in this phase. Critical features like patient management, clinical documentation, and security requirements are identified here. The discovery phase sets the foundation for a tailored solution.
- Design and Architecture Planning: Developers and designers create a system blueprint during this phase. This blueprint outlines the data flow, interfaces, and integration points with other healthcare systems, such as lab databases or pharmacy management software. The healthcare architecture must be scalable and secure to handle sensitive data effectively.
- Implementation and Testing: Once the design is approved, development begins. The software development team builds the system’s core functionalities using the chosen tech stack. QA testers work alongside the developers to ensure the system meets the defined requirements and is bug-free. Rigorous testing also ensures that the system can handle large volumes of data without compromising speed or security.
- Deployment: After testing the development of EHR systems; during this phase, healthcare staff are trained to use the system effectively. A go-live strategy ensures a smooth transition from old systems to the new EHR platform. Post-launch support is crucial for addressing issues and ensuring the system functions as expected in real-world use.
Related reading: Software Architecture for Healthcare Apps
Final Takeaway
To contribute to the success of feasible and convenient healthcare facilities, EHR system development has repeatedly proven to be more than just digital repositories for medical records. They represent a transformative step capable of revolutionizing patient care and enhancing medical outcomes. From automating workflows to integrating AI for predictive healthcare, the potential of developing EHR software systems is limitless. As interoperability and personalized medicine become the norm, the impact of EHR systems on healthcare will continue to grow, improving both the efficiency of medical institutions and the quality of patient care.If you’re a healthcare provider in Canada looking to leverage these advancements and create an EHR system tailored to your specific needs, AppStudio is your go-to partner. With a deep understanding of healthcare IT and a proven track record of delivering secure, scalable solutions, AppStudio is uniquely positioned to help you design and implement the next generation of EHR software that aligns with your goals and meets the evolving demands of modern healthcare. Schedule a FREE Consultation today.
Frequently Asked Questions
EHR stands for Electronic Health Record provides a comprehensive view of a patient’s health, accessible across different healthcare providers and settings, while EMR stands for Electronic Medical Record focuses on individual clinic data and is not easily shared outside that clinic.
The timeline for EHR software system development varies depending on its complexity. On average, it can take 6 months to 18 months, factoring in initial planning, development, testing, and deployment stages.
A cloud-based EHR offers flexibility, lower upfront costs, and easier scalability, making it ideal for smaller practices. On-premise systems provide greater control and customization but require significant IT resources and maintenance, often better suited for larger organizations.
EHR systems must include encryption (AES-256), multi-factor authentication (MFA), and role-based access control (RBAC). These measures help protect sensitive patient data from breaches, ensure compliance with regulations like HIPAA, and maintain system integrity.
Yes, EHR software system development are can be integrated with other healthcare platforms like lab systems, pharmacy management software, and billing tools. This is achieved through APIs and interoperability standards like FHIR.
In the US, EHR systems must comply with HIPAA to ensure data privacy and security. In Europe, GDPR applies. Compliance ensures patient data is protected, and legal risks are minimized.
Yes, EHR systems can be fully customized to meet the specific workflows of different healthcare practices, such as specialized treatments in oncology or cardiology. Custom-built EHRs allow for greater flexibility and integration with specialized tools.